https://www.infirmiere-canadienne.com/blogs/ic-contenu/2025/09/29/stigmatisation-lire-poids-dans-systeme-sante
How health professionals can address a person’s weight with compassion
By Jenny Lambert, Maude Plouffe, & Anne-Marie Leclerc
September 29, 2025
 istockphoto.com/andreswd
istockphoto.com/andreswd
Nursing staff must offer and promote care free from weight-related stigma. Doing so will help ensure that nurses are better equipped to intervene with clients and promote healthy lifestyles rather than focus exclusively on weight reduction.
Takeaway messages
- There are different forms of weight-related stigma. Although the intentions are often well-meaning and focus on health concerns, many attitudes and behaviours are stigmatizing.
- There are numerous impacts to those who are the victims of victims weight-related stigma.
- Nurses have a crucial role to play in countering weight-related stigma in the health-care system.
Weight-related stigma refers to negative attitudes and beliefs associated with weight, manifested through stereotypes, rejection, and prejudice towards people based on their weight (Puhl et al., 2008). These authors argue that it is one of the most widespread and socially accepted forms of stigma. Health professionals can exhibit stigmatizing behaviour towards patients, which can manifest as judgments, inappropriate comments, and excessive focus on weight leading to under-investigation or over-investigation — or even shorter appointments — for individuals with higher weight (Puhl, 2023).
One recent study revealed that 60% of people with obesity have experienced weight stigma during their medical care (Wharton et al., 2020). This statistic is concerning considering that stigma is linked to a decrease in the quality of care by health professionals, as well as to avoiding consultations, decreased motivation, and adherence to treatments by patients (Puhl, 2023). Weight stigma can take many forms (Association pour la santé publique du Québec, 2024; Bernier, 2023), including:
- Unconscious biases and prejudices (regardless of one’s weight) and the culture of blame for one's weight status
- Use of facilities and infrastructure that are not adapted to a wide range of body styles (e.g., narrow waiting room seats)
- Judgment of a person based on their weight and attribution of negative traits to them (e.g., laziness and reduced worth)
- Unsolicited advice that comes from good intentions, often related to health concerns for the person
- Implication/hints that people who are higher weight are unattractive
- Belief that fighting against weight-related stigma promotes obesity
- Justifification of the validity of one’s prejudices as beneficial to society (in terms of health-care costs)
The impacts of weight-related stigmatization
People with higher weight tend to report greater body dissatisfaction than those whose weight aligns more closely with societal norms (Aimé et al., 2022). Indeed, the impacts of body dissatisfaction are detrimental to mental health, and scientific literature on the subject reveals that women are more affected (Rodgers et al., 2023; Gualdi‐Russo et al., 2022).
It is important to remember that a person’s weight is influenced by multiple factors, many of which are beyond their control (Wharton et al., 2020). These include heredity and genetics, the individual’s health, the social and physical environment in which they live, and their socioeconomic status. In short, a person's body size is not determined by their will or worth; it is rather influenced by many often uncontrollable factors.
Yet, people with higher weight are often targets of stigmatization and discrimination. Several empirical studies show that the impacts of weight-related stigmatization can affect various aspects of health (Alberga et al., 2019; Mensinger et al., 2018). These impacts are numerous and create health disparities by engendering, amongst others, the following risks:
- Increase in stress levels / chronic stress
- Increase in concerns about appearance
- Increased risk of developing eating disorders
- Avoidance of physical activity
- Avoidance of health-care professionals
- Increased risk of psychological distress
- Increased risk of mortality
The following figure shows the various impacts of weight-related stigma that can, ironically, lead to additional weight gain.
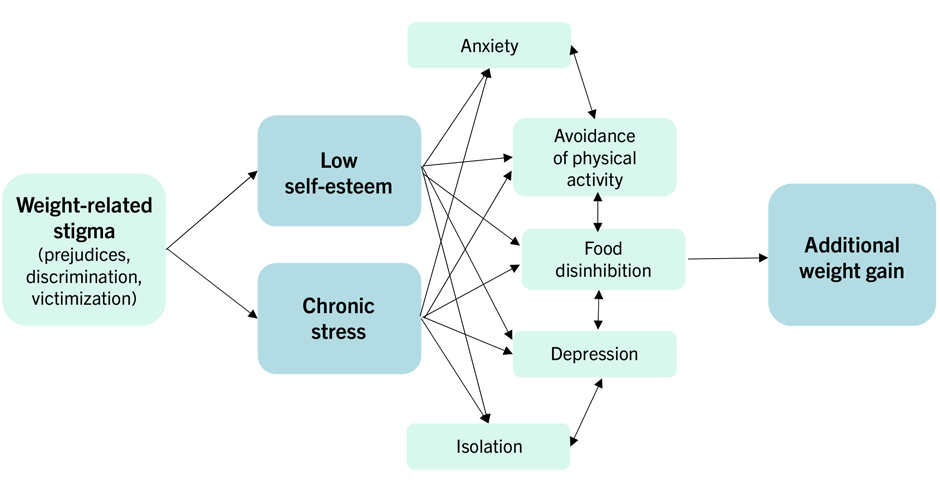 Impacts of stigma on weight management, Adaptation from Albury et al., (2020)
Impacts of stigma on weight management, Adaptation from Albury et al., (2020)
Body prejudices may be wrongly perceived as adequate or even necessary to motivate a person to change their lifestyles to address their higher weight. Making people believe they have full control over their weight has the adverse effect of inducing guilt and, thereby, hindering the adoption of health-promoting behaviours. Indeed, Zhu et al. (2022) report that weight stigma is negatively associated with health-promoting behaviours and positively associated with health-harming behaviours.
The role of nurses in tackling and addressing weight-related stigma
Quebec’s public health association (Association pour la santé publique du Québec, 2024) proposes solutions to tackle weight-related stigma against people with higher body weight, such as: 1) becoming aware of one’s beliefs and prejudices regarding weight; 2) nuancing the link between weight and health; 3) using inclusive and non-stigmatizing language; 4) training health professionals on weight-related issues; 5) not tolerating discriminatory behaviours; and 6) adapting medical equipment to different body sizes. Additionally, the association also recommends the use of respectful images in communications.
To address weight in a compassionate manner, the Obesity Canada 2020 guidelines recommend five steps to guide health professionals in their intervention with a person with higher weight.
- Recognize obesity as a chronic disease, instead of placing the blame personally on the patient, and ask the person for permission to discuss their weight. Establishing a trustful relationship is essential for communication; it can help you understand the situation that led to weight gain determine how to intervene appropriately.
- Assess the patient and consider the individual’s experience and life goals ; doing so can help you identify potential motivational levers and contributing factors (e.g., obesogenic medications). To assess the severity of obesity and its health impacts, use the Edmonton Obesity Staging System (EOSS) rather than the body mass index (commonly known as BMI), which is not reliable enough to identify complications related to obesity. The EOSS takes into account metabolic, physical, and psychological factors to develop an adapted treatment plan.
- Discuss therapeutic options that consider the user's experience.
- Develop a long-term action plan in collaboration with the individual. As with all chronic diseases, the first level of intervention is the improvement or maintenance of healthy lifestyle habits for all individuals, regardless of their weight.
- Ensure follow-up and promote obesity treatment. Evidence-based continuing education and support for access to health resources for effective obesity treatments (behavioural, pharmacological, and surgical) are recommended.
In conclusion, nursing staff must offer and promote care free from weight-related stigma. Doing so will help ensure that nurses are better equipped to intervene with clients and promote healthy lifestyles rather than focus exclusively on weight reduction.
The path for the future
It would be interesting to further explore the issue of weight-related stigma within the nursing profession, especially in research to better understand the specific manifestations of stigma in the nursing field, whether in the form of implicit judgments, stereotypes, or discriminatory behaviours. Such an approach could help identify risk factors — whether personal, institutional, or social — that contribute to these manifestations.
At the same time, it would be essential to develop strategies to eliminate weight-related stigma in nursing practice. One of the first steps is to raise awareness among health-care professionals about their own biases; this helps individuals become aware of their conscious and unconscious prejudices.
Additionally, implementing specific training on obesity and weight-related stigma would complement the guidelines proposed by Obesity Canada.
Finally, it is pertinent to consider systematic interventions, such as prejudice deconstruction workshops or institutional policies, to foster an inclusive care culture within health-care facilities. These actions could serve as a lever to promote an environment where body diversity is not only accepted, but also respected.
References
Aimé, A., Dion, J. & Maïano, C. (2022). L’image corporelle sous toutes ses formes [Body image in all its forms]. Presses de l’Université du Québec. https://www.puq.ca/catalogue/themes/image-corporelle-sous-toutes-ses-formes-3573.html
Alberga, A. S., Edache, I. Y., Forhan, M., & Russell-Mayhew, S. (2019). Weight bias and health care utilization: a scoping review. Primary Health Care Research & Development, 20, e116. https://doi.org/10.1017/S1463423619000227
Albury, C., Le Brocq, S., Lloyd, C., Strain, D., & Logue, J. (2020). Language matters: obesity. https://icpobesity.org/wp-content/uploads/2021/10/Obesity-UK-Language-Matters-2020.pdf
Association pour la santé publique du Québec & Coalition québécoise sur la problématique du poids. (2021). Groupe de travail provincial sur les problématiques du poids pour des communications saines sur les problématiques reliées au poids. https://collectifvital.ca/files/P2-Enjeux_poids/Rapport_GTPPP.pdf
Bernier, E. (2023). Grandir sans grossophobie : favoriser une image corporelle saine chez nos enfants. Éditions du Trécarré.
Gualdi‐Russo, E., Rinaldo, N., Masotti, S., Bramanti, B., & Zaccagni, L. (2022). Sex differences in body image perception and ideals: Analysis of possible determinants. International Journal of Environmental Research and Public Health, 19(5), 2745. https://doi.org/10.3390/ijerph19052745
Mensinger, J. L., Tylka, T. L., & Calamari, M. E. (2018). Mechanisms underlying weight status and healthcare avoidance in women: A study of weight stigma, body-related shame and guilt, and healthcare stress. Body Image, 25, 139-147. https:// doi.org/10.1016/j.bodyim.2018.03.001
Puhl, R. M., Moss-Racusin, C. A., Schwartz, M. B., & Brownell, K. D. (2008). Weight stigmatization and bias reduction: Perspectives of overweight and obese adults. Health education research, 23(2), 347-358. https://pubmed.ncbi.nlm.nih.gov/17884836/
Puhl, R. M. (2023). Weight stigma and barriers to effective obesity care. Gastroenterology Clinics, 52(2), 417-428. https://doi.org/10.1016/j.gtc.2023.02.002
Rodgers, R. F., Laveway, K., Campos, P., & de Carvalho, P. H. B. (2023). Body image as a global mental health concern. Global Mental Health, 10. https://doi.org/10.1017/gmh.2023.2
Wharton, S., Lau, D. C. W., Vallis, M., Sharma, A. M., Biertho, L., Campbell-Scherer, D., … Wicklum, S. (2020). Obesity in adults: a clinical practice guideline. Canadian Medical Association Journal, 192(31), 1775. https://doi.org/10.1503/cmaj.191707
Zhu, X., Smith, R. A. et Buteau, E. (2022). A meta-analysis of weight stigma and health behaviors. Stigma and Health, 7(1), 1-13. https://doi.org/10.1037/sah0000352
Acknowledgements
The authors warmly thank professors Marie-Pierre Gagnon-Girouard and Noémie Carbonneau for their valuable advice and for reviewing this article.
Jenny Lambert, RN, B.Sc., is a master’s student in nursing at the Université du Québec à Trois-Rivières (UQTR), is a primary care nurse, and is a member of the professional committee of Diabète Mauricie.
Maude Plouffe is a doctoral student in psychology (D.Psy.) at UQTR.
Anne-Marie Leclerc, RN, PhD is an associate professor in the nursing department at UQTR.
#analysis
#chronic-conditions
#clinical-practice
#food-nutrition
#nurse-patient-relationship
#nursing-practice
#patient-experience