https://www.infirmiere-canadienne.com/blogs/ic-contenu/2025/09/02/introduction-pouvoir-prescription-ontario
Article and framework aim to support other jurisdictions as they navigate the complexities of expanding RN scope of practice
By Treva Job, Jessica Milligan, & Sara Lankshear
September 2, 2025
 istockphoto.com/mixetto
istockphoto.com/mixetto
Learning to diagnose and prescribe medications within the RN’s scope of practice is a steep learning curve. For anyone who finds themselves pioneering a new role, it means there will be kinks and bumps along the way, some unanticipated and therefore requiring further exploration and integration.
Although recently introduced in Ontario, RN prescribing is not new to Canada. The Canadian Nurses Association (CNA) published the Framework for Registered Nurse Prescribing in Canada 10 years ago. The three fundamental, interdependent elements grounding the Canadian framework are structure, competence and practice (CNA, 2015).
The current state of RN prescribing in Canada indicates that there are six provinces in Canada that authorize RN prescribing – Alberta, British Columbia, Manitoba, Nova Scotia, Prince Edward Island, and Quebec – with each province having unique practice standards, guidelines, and educational requirements (British Columbia College of Nurses & Midwives, 2020; Cole, 2018; College of Registered Nurses of Manitoba, 2018; Menard & Trudeau, 2015; Moody et al., 2025; Saskatchewan Registered Nurses Association, 2018).
Although our work as educators at Georgian College, which offers one of the first RN prescribing programs in Ontario, is grounded in Ontario regulations, the strategies, considerations and information here are broadly applicable and can inform educators, regulators, and nursing leaders across jurisdictions in Canada.
This article shares lessons learned from Georgian College as we traversed delivery of the RN prescribing curriculum within the first year of RN prescribing in Ontario. By highlighting aspects of our experience, we aim to support others as they navigate the complexities of introducing RN prescribing education in their own regions and jurisdictions across Canada.
RN prescribing in Ontario
In November 2023, the Ontario government passed legislative changes to the Nursing Act, 1991, that permit RNs to prescribe certain medications and communicate diagnoses for purposes of prescribing. In June 2025, Ontario announced funding for nursing education, investing $750,000 to support the inclusion of RN prescribing in three undergraduate nursing programs, Georgian College being one of them. This will make Ontario the first jursidiction in Canada to include RN prescribing in undergraduate programs beginning in the 2025-26 academic year.
Under this regulation, RNs must complete a College of Nurses of Ontario (CNO)–approved educational program (CNO, 2024), as RN prescribing is currently not part of the entry-to-practice competencies. RNs with the authority to prescribe can only do so in practice settings or facilities where RN prescribing is authorized by law and permitted by the employer (CNO, 2024). In addition, the current regulation outlines the list of approved medications: immunization, contraception, travel health, topical wound care, smoking cessation, anesthetics, allergic reaction and over-the-counter medication (CNO, 2024).
Employers are responsible for determining the roles and responsibilities of their employees. RNs are expected to consult with their employers to understand and confirm whether they are permitted to prescribe. The College of Nurses of Ontario RN prescribing practice standard is based on three key principles: authority, competence and safety (CNO, 2024). All nurses are accountable to comply with the laws, CNO standards and guidelines that apply to all nursing practices; this extends to RNs authorized to prescribe (CNO, 2024).
A framework to support RN prescribing
To inform the development of our RN prescribing curriculum, we first reviewed the literature. Our review revealed an important gap: there was no clearly defined framework that captured the prescribing process necessary for guiding safe and ethical prescribing practices. There is a paradigm shift required to fully conceptualize the process of formulating a diagnosis for the purpose of prescribing a medication then determining the appropriate medication. To address this gap, we developed a framework (Figure 1) to inform safe and ethical RN prescribing.
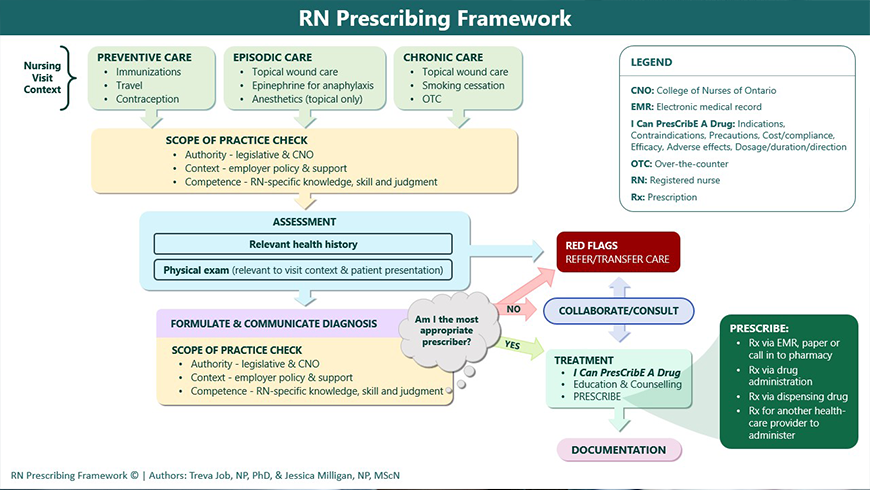 Figure 1. RN Prescribing Framework
Figure 1. RN Prescribing Framework
Georgian College’s RN prescribing program
The RN Prescribing Framework has been used as the foundational component of Georgian College’s safe and ethical RN prescribing curriculum. The framework assists the RN prescriber to consider the context of the visit to conceptualize the type of care that may be required. Diagnosis takes place after a thorough assessment, which includes relevant history – including a best possible medication history – and the appropriate physical assessment. At any given time within the encounter, the RN is required to rule out any red flags and determine if the care needs identified are within the scope of the RN prescriber or whether they require consultation or a complete transfer of care to another prescriber. Choosing a treatment plan requires reviewing patient-specific factors and having a thorough understanding of medications used to treat that clinical indication. RNs also need to consider, throughout the encounter, if they are the most appropriate prescriber within the context of that patient, the clinical indication, and the specific medication.
Based on feedback from new RN prescribers, learning to diagnose and prescribe medications within the RN’s scope of practice is a steep learning curve; therefore, having a practical RN prescribing framework provides a useful guide to clarify expectations of the RN prescribing process.
Georgian College offers the Registered Nurse Prescribing Education Program: Safe and Ethical Practice, which includes both a theory and a clinical practicum component. The theory component consists of four modules: professional responsibilities and accountabilities; professional and ethical responsibilities; assessment and diagnosis; and pharmacotherapy and other therapeutic interventions in client care (the subsections within module 4 are specific to the current RN prescribing list of medications authorized in Ontario).
To support the immediate adoption of prescribing, the program admission criteria require a letter of support from candidates’ employers and proof of a clinical/prescribing mentor (nurse practitioner or physician) who would support their practicum component.
The practicum component includes submission of prescription logs, patient/client-specific care plans, and a quality assurance learning plan with identified goals. There are multiple opportunities for feedback from faculty throughout the clinical practicum, as this is an integral part of the learning transition from the role of the RN to the role of the RN prescriber.
RN prescribing students
Upon registration and before initiating the course content, a voluntary demographic survey is offered to all students enrolled in the program. Based on survey results from the initial cohort, students had 1 to 37 years of experience, with an average of 12 years. Many of the students had completed a registered practical nurse (RPN) to RN bridge program and previously worked as an RPN.
In our first cohort we noted that RNs with more than 10 years of experience demonstrated stronger clinical judgment and decision-making skills than students with less experience. This was also evident in the quality of the clinical practicum assignments submitted, such as detailed assessments and plans of care. Further research is required to explore these relationships in more detail.
Students shared that some of their perceived benefits of RN prescribing included contributing to increasing efficiency, effectiveness, continuity, and improved quality of care for their clients. Like the vision of CNA (2015), and as described by Darvishpour et al. (2014), many of the RNs in our program felt that having the autonomy and independence to prescribe for their clients improved workflow, especially direct client care, without delays in treatment. Our students were an exceptionally motivated, dedicated and passionate group of RNs who were eager to address barriers and gaps in their clients’ health-care needs and pioneer this role in Ontario.
Lessons learned in nursing practice
When considering the successful adoption and implementation of RN prescribing in the various practice settings, two themes emerged: role clarity and organizational support.
Role clarity for the prescriber
Learning to diagnose and prescribe medications within the RN’s scope of practice is a steep learning curve. This is where our students found the RN Prescribing Framework beneficial, as it assisted in clarifying the expectations of the RN prescriber practice. On several occasions students, mentors and faculty collaborated to navigate, negotiate and truly understand the complexities, detailed intricacies, and nuances of this new scope of practice for RNs.
For anyone who finds themselves pioneering a new role, it means there will be kinks and bumps along the way, some unanticipated and therefore requiring further exploration and integration. A common phrase that was often stated when coaching and mentoring the RNs enrolled in the program was, “just because you can, doesn’t mean you should.” This was instrumental in helping RNs develop further and deepen their understanding of their role while helping to ensure safe and ethical prescribing practices. We also worked closely with regulators to clarify the RN prescriber role; as such, the regulator was able to more clearly address the clinical indications and medications specific to RN prescribers in Ontario.
Role clarity for the employer
Employers and organizations must be willing to provide the appropriate support for RNs authorized to prescribe to meet the standards of practice and requirements for self-regulation. In the initial cohort of RN practice settings that were early adopters of RN prescribing, there was a need to develop and implement policies and procedures specific to RN prescribing. This included, but was not limited to developing an evidence-informed guidance document detailing the parameters for the role of the RN prescriber for the identified area of need. This was done in consultation with early-adopter practice settings applying for authorization to prescribe.
Evidence-informed clinical decision tools are used by RN prescribers to help guide specific RN prescribing practice decisions for a specific clinical indications, medications and populations. These clinical support tools may take the form of a protocol, algorithm, policy or clinical practice guideline that is supported by the employer and meant to help manage risk and clinical expectations for the novice RN prescriber (Moody et al., 2020; Saunders, 2021).
Employer responsibility includes having clear policies and procedures in place for their interprofessional team, as the lack of these could potentially create problems in the event of liability. Other considerations that were identified in the literature to help navigate this shift in practice effectively include but are not limited to the following:
- Quality assurance (CNO, 2024) and practice considerations related to ongoing monitoring and evaluation of patient outcomes, patient safety, and health-care delivery within your organization (CNA, 2015)
- Championing evidence-based practice, promoting interdisciplinary collaboration and advocating for policies that support expanded roles for RNs in medication management (CNA 2015)
- Evaluation and feedback related to the implementation of the registered nurse prescriber within your organization (CNA, 2015).
Conclusion
We have learned several key lessons that may support other provinces and territories embarking on similar initiatives.
- Collaboration is essential: Strong partnerships between education, practice and regulatory bodies are critical to ensure alignment with professional standards and safe and ethical prescribing practices.
- Context matters: When foundational prescribing principles are consistent, curriculum design and delivery methods must be adaptable and inclusive to advance practice.
- Frameworks and tools: Embedding prescribing content, tools and frameworks with broader clinical and decision-making processes reinforces critical thinking and professional accountabilities while helping RNs gain confidence in their prescribing competency.
- Iterative refinement supports growth: Ongoing evaluation and feedback allows for curriculum responsiveness and improvements as RN prescribing evolves and expands in the practice environment.
References
Canadian Institute for Health Information. (2022). Registered nurses. https://www.cihi.ca/en/registered-nurses
Canadian Nurses Association. (2015). Framework for registered nurse prescribing in Canada. https://hl-prod-ca-oc-download.s3-ca-central-1.amazonaws.com/CNA/2f975e7e-4a40-45ca-863c-5ebf0a138d5e/UploadedImages/documents/CNA_RN_prescribing_framework_e.pdf
College of Nurses of Ontario. (2024). Practice standard: Registered nurse (RN) prescribing. www.cno.org/globalassets/docs/prac/practice-standards-rn-prescribing.pdf
Darvishpour, A., Joolaee, S., & Cheraghi, M.A. (2014). A meta-synthesis study of literature review and systematic review published in nurse prescribing. Medical Journal of the Islamic Republic of Iran, 28(77). https://pmc.ncbi.nlm.nih.gov/articles/PMC4219909/
Government of Ontario. (1991). The nursing act: Ontario regulation 275/94. https://www.ontario.ca/laws/regulation/940275#BK41
Moody, E., Martin-Meisener, R., Carrier, J., MacDonald, M., MacMillan, K., & Axe, S. (2020). The educational terrain of preparing registered nurses to prescribe: An environmental scan. Nursing Research, 33(2)., 54-67. doi:10.12927/cjnl.2020.26237
Ontario Public Hospitals Act. (1991). https://www.ontario.ca/laws/statute/90p40
Saunders, M. M. (2021). Informing and supporting the new clinical nurse specialist prescriber, AACN Advanced Critical Care, 32(4), 404-412. doi:10.4037/aacnacc2021869
Treva Job, PhD, RN, PHC-NP, M.A.Ed., CCSNE, is manager of the simulation centre at Georgian College and has over 28 years of nursing experience.
Jessica Milligan, RN, MN, PHC-NP, has over 20 years of diverse nursing experience, including 11 years as both a primary health care nurse practitioner and part-time nursing faculty with Georgian College.
Sara Lankshear, PhD, RN, FCAN, is the associate dean of nursing programs at Georgian College and has been an educator for 20 years.
#practice
#clinical-practice
#health-system
#interprofessional-collaboration
#nursing-education
#nursing-practice
#patient-care